T. Bendeliani
Medical Corporation "Evex", Tbilisi, Georgia
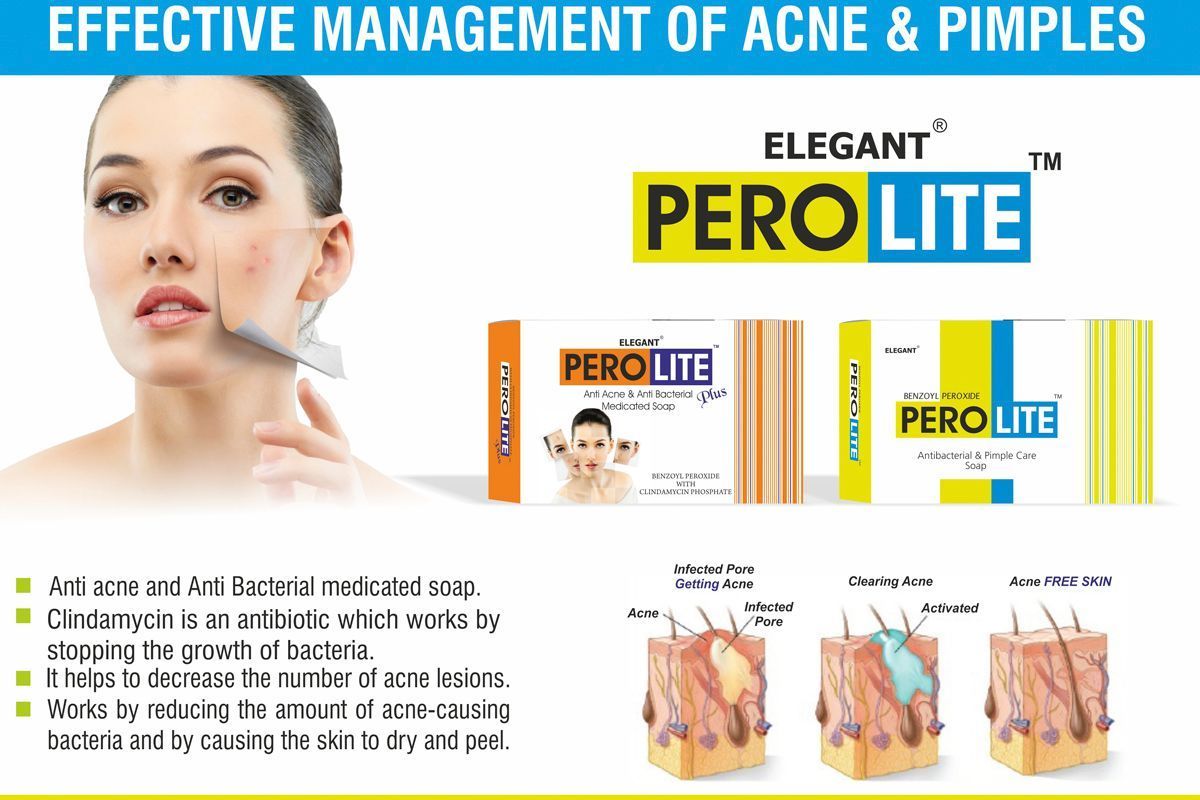
The data of a clinical study of the effectiveness of soap with the brand name "Perolait", which contains benzoyl peroxide, and "Perolait Plus", which contains benzoyl peroxide and clindamycin, for the topical treatment of acne are presented.
The studies conducted in clinics in Georgia from May 2017 to April 2018 involved 120 patients with mild to moderate acne (according to the Dermatological Acne Index). Perolite and Perolite Plus soaps were used twice a day (morning and evening) as monotherapy in patients with mild acne and in combination with a gel containing benzoyl peroxide in severe cases.
After just 1 month of using the soap, most patients (83%) with mild disease severity showed a decrease in the dermatological acne index, while in patients with moderate disease severity, the index decreased by more than 60%.
Especially rapid improvement occurred when using Perolite Plus soap in patients with pronounced pustular elements. Based on the results of the study, it can be concluded that Perolite soap has sufficient therapeutic activity and is well tolerated by patients when conducting both mono- and complex acne therapy.
In addition, it can be successfully used in the summer. All this gives reason to recommend Perolite soap for widespread use in clinical practice.
Keywords: Acne, Perolite soap, benzoyl peroxide.
Acne is a polymorphic multifactorial disease characterized by genetic predisposition. According to statistics, it is the most common skin pathology among dermatoses - acne affects up to 85% of people aged 12 to 25 years [2]. It is an extremely common phenomenon, especially among residents of megacities, who are more susceptible to the negative effects of environmental factors.
Acne affects approximately 85% of adolescents (of which 25% have severe disease). Active forms of acne are diagnosed in 20% of adults, and approximately 50% of women regularly experience outbreaks of rashes. Acne belongs to a group of diseases called psychosomatic dermatoses, which are associated with the problem of "appearance defect", reduce a person's self-esteem and are a cause of depression and anxiety. Despite the availability of modern treatment methods, acne still remains one of the most common dermatoses - its incidence not only does not tend to decrease, but also increases markedly.
The pathogenetic factors for the development of acne include:
- hypersecretion of the sebaceous glands,
- change in the qualitative parameters of sebum and epidermal lipids;
- pathological keratinization of the follicular canal in the infundibular part (between the sebaceous gland and the surface of the epidermis);
- intensive colonization of Propiono bacterium acnes in the sebaceous glands;
- development of an inflammatory reaction in the perifollicular zones [1].
In some cases, topical agents are the first line of acne treatment, especially at the beginning of the disease and in mild forms of acne vulgaris. In 2002, recommendations were developed and an algorithm for pathogenetic treatment of patients with various forms of acne was created (XX World Congress of Dermatology, Paris, 2002), in which the first-choice drugs are local retinoids, benzoyl peroxide, antibiotics and azelaic acid, which affect the processes of keratinization (keratinization and desquamation), reduce sebum secretion, increase the proliferation of skin epithelial cells and have a certain anti-inflammatory effect [4].
Today, one of the effective ways to treat acne is benzoyl peroxide, which contains a benzoic acid residue. When applied to the skin, this lipophilic compound enters into a chemical reaction with oxygen and breaks down into two substances - peroxide and benzoic acid. The latter substance is not active and is not absorbed into the skin. Active peroxide destroys bacteria by affecting their walls, and also reduces the level of fatty acid secreted by the skin, thereby preventing the occurrence of inflammation. In addition, the agent has a therapeutic effect - it damages keratinized cells and prevents skin peeling.
Benzoyl peroxide exhibits nonspecific antimicrobial activity against P. acnes, Staphylococcus epidermidis and some other microorganisms and has been used in dermatology since the 20th century. [3]. Being a powerful oxidant, it penetrates follicles better than other local agents, contacts the P. acnes membrane and has a bactericidal effect. When benzoyl peroxide is destroyed, benzoic acid is formed, which acts bacteriostatically, does not accumulate in tissues, does not have a systemic effect and is excreted unchanged from the body. The anti-inflammatory effect of benzoyl peroxide is due to the inactivation of free radical oxygen species in the focus of inflammation, the destruction of free fatty acids and a decrease in their concentration. The comedonolytic effect of benzoyl peroxide is explained by the fact that, according to its chemical structure, it is a strong oxidant that suppresses the inflammatory process and the formation of comedones [4].
The advantage of drugs containing this substance is that they do not cause the emergence of resistant strains of bacteria.
120 patients with acne were monitored for a year, the severity of which was determined taking into account the number of comedones, pustules, papules and nodules. In the presence of single elements, the dermatological acne index was less than 5 points (mild severity), in the presence of a moderate number - 6-15 points (moderate severity), in the presence of a large number - more than 15 points. Mild severity was diagnosed in 78 (65%) patients and moderate severity in 42 (35%). For mild acne, Perolite soap was prescribed twice a day (morning and evening) as monotherapy and in combination with a gel containing benzoyl peroxide. In this case, patients used the soap in the evening and the gel in the morning. Regardless of the severity of the process, but in the presence of multiple pustular elements, Perolite plus soap containing clindamycin was prescribed.
The average course of treatment in most cases was 5-7 weeks. Only in three patients with moderate acne severity the course was extended to 8-9 weeks. The effectiveness of therapy was assessed by the change in the dermatological acne index 1 month after the start and 6-8 weeks after the end of treatment.
The safety of Perolite soap, objective and subjective data on effectiveness, and the dynamics of the clinical course of acne during treatment were analyzed.
After 1 month of using the soap, most patients with mild acne showed a decrease in the dermatological acne index (83%), with moderate severity the index decreased by more than 60%. Especially rapid improvement occurred when using "Perolait Plus" in patients with pronounced pustular elements. All patients tolerated the soap well: 80% of them rated the tolerance as very good, 20% - as good. An important point was the absence of side effects associated with insolation in the summer. All patients with mild acne noted the effectiveness of the soap as very good and were completely satisfied with the results of the treatment. Most patients with moderate acne were satisfied with the results of the treatment, only in 3 cases it was not possible to achieve a full clinical effect within 2 months. It is also important that the quality of life of patients with acne is one of the factors of effectiveness, since the disappearance of clinical manifestations has a beneficial effect on their general and mental state.
Based on the results of the study, it can be concluded that Perolite soap has sufficient therapeutic activity and is well tolerated by patients when conducting both mono- and complex acne therapy. In addition, it can be successfully used in the summer. All this gives reason to recommend Perolite soap for widespread use in clinical practice.
References
1. Kiselyova N.V. The role of histocompatibility antigens in the development of various forms of acne and methods of correction: author's abstract of the dissertation ... candidate of medical sciences; 14.00.11.- M., 2001.- 22 p.
2. Cunliffe WJ New Approaches To Acne Treatment.- London: Martin Dunitz, 2004.- 56 p.
3. Perry A., Lambert P. Propioni bacterium acnes: Infection beyond the skin // Expert Review of Anti-infective Therapy.- 2011.- Vol. 9, N 12.- P. 1149-1156. doi: 10.1586 / eri.11.137.
4. Savage LJ, Layton AM Treating acne vulgaris: systemic, local and combination therapy // Expert Rev. Clin. Pharmacol.-2010.- Vol. 13.- P. 563-580. doi: 10.1586 / ecp.10.27.
5. Zaenglein AL, Pathy AL, Schlosser BJ et al. Guidelines of care for the management of acne vulgaris // J. Am. Acad. Dermatol.- 2016.- Vol. 74, N 5.- P. 945-9 73. doi: 10.1016 / j. jaad. 2015.12.037.